Don't Fall Behind on Your Notes
Quickly turn your shorthand, dictation , sessions , telehealth and recordings into SOAP notes. Works with any healthcare specialty.
Save time with our HIPAA-compliant AI documentation assistant.
HIPAA-Compliant
No credit card required to start
SOAP Note For All Healthcare Specialties
Saving time for 1000s of therapists, physical therapists, nurse practitioners, occupational therapists, social workers, SLPs, registered nurses and other healthcare professionals.
- Users
- 0
- SOAP Notes Generated
- 0
- Hours Saved
- 0
What Healthcare Professionals Say About SOAPNoteAI
Loved by healthcare professionals.
Hear from real clinicians who save time by using SOAP Note AI.
SOAPNoteAI.com was particularly helpful during a busy clinic day when I had to see a high volume of patients. It allowed me to quickly generate accurate SOAP notes for each encounter, saving me considerable time and reducing the risk of errors.
Dr. Todd Carman-WagnerPh.D., DSW-LICSWI LOVE SOAP Note AI! It gives me back the time that charting was taking away from my patients at work and my family at home. I am so grateful for this tool and use it for every session, every day!
Allison CarrollMental Health ProfessionalSOAP NOTE AI is definitely a time saver and improves the quality of my clinical notes to ensure they meet clinical guidelines. Discovering your company via Facebook was the best find of my career.
Dr. GregLCSW, PMHNP-BCGetting my notes done on time was a challenge but it's been extremely useful to have this tool and have timely notes completed.
Dr. Samara ToussaintPath2Growth CounselingSOAP Note AI gives me continuity of patient charts and more extensive coverage regarding risk, patient care, follow up, etc. that offers thorough professional statements.
J.R.Nurse PractitionerSOAP Note AI has improved my quality of life, completing notes faster and with ease, spending more time with my family. It is a huge game changer.
G.M.PMHNPSOAPNoteAI helps address time constraints relating to taking partial notes from sessions and maximizing my time to see more clients.
SOAP Note AI customerDoctor of PsychologySOAPNoteAI does a great job of helping me process vital information in my professional notes and gives me key insights on how to write them up correctly.
Eric CarpenterPsychotherapy ProfessionalI recall a session where the client's diagnosis did not quickly jump out at me. SoapNoteAI was able to quickly come up with a diagnosis based on the symptoms I provided. It saved me time and headache.
Julio ColonMental Health Professional
Trusted by 1000+ healthcare professionals
Tired of Staying Late for Documentation?
You're not alone. 73% of healthcare professionals report documentation burnout. Your evenings and weekends deserve better.
Get your life back in under 10 minutes • See real success stories
Healthcare Professions We Support
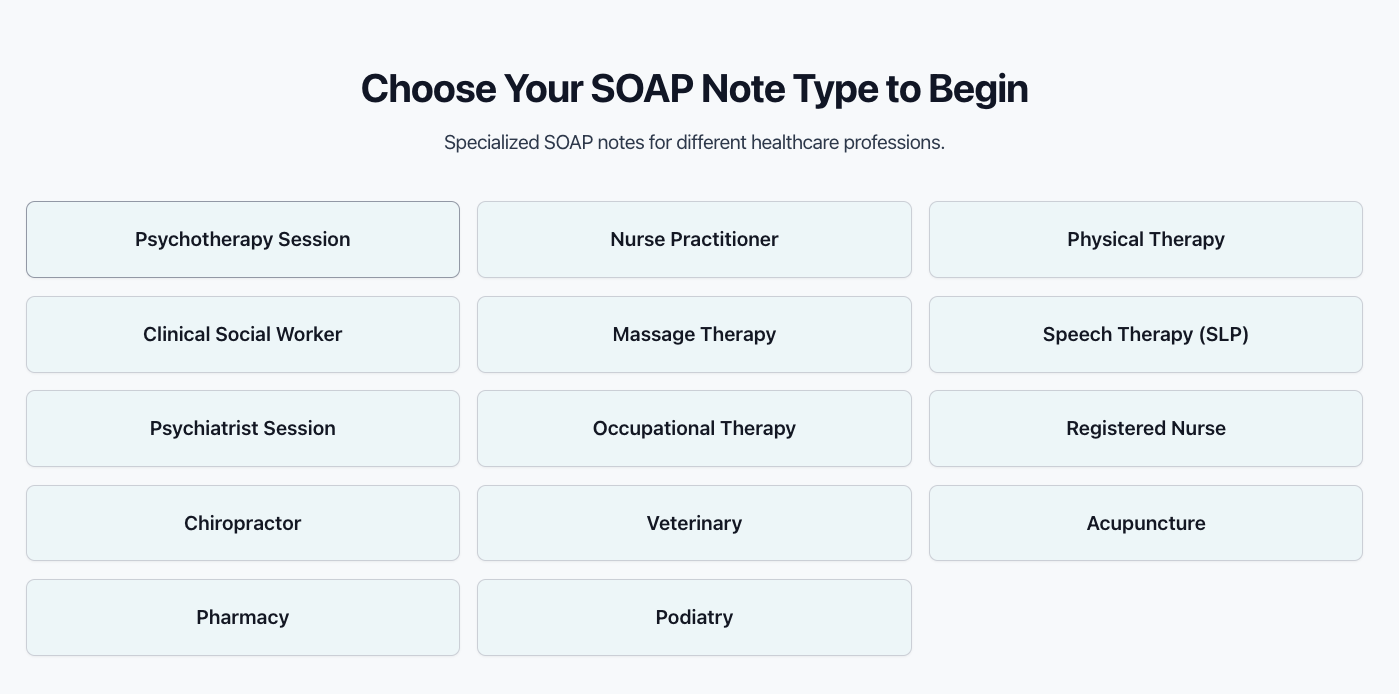
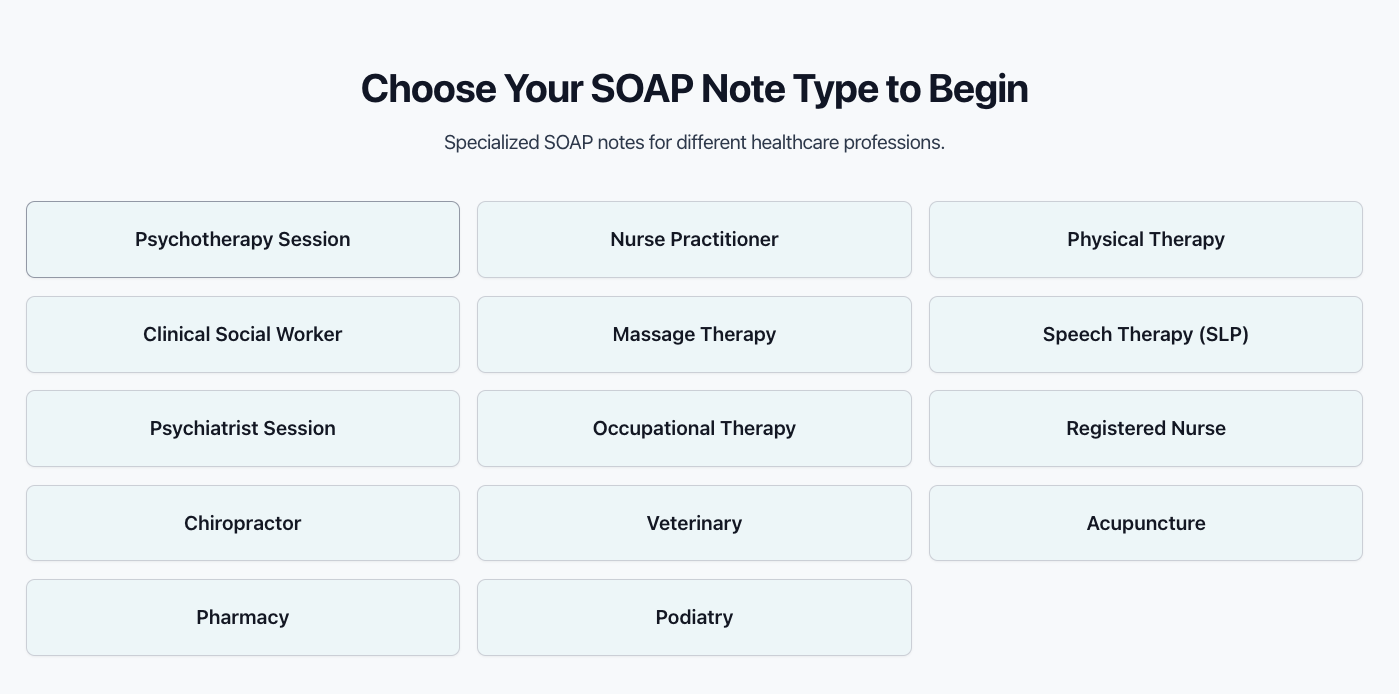
Choose Your SOAP Note Type to Begin
Specialized SOAP notes for different healthcare professions.
Cannot find what you are looking for?
Email us at support@soapnoteai.com to request your SOAP note type.
Can SOAP Note AI help with CYBHI?
Yes, Please click here to learn more.
Key Features of SOAPNoteAI
Save Time with SOAP Note AI
Generate detailed SOAP notes effortlessly from your shorthand, dictation, telehealth sessions or record a session.
Quickly convert your shorthand notes into comprehensive SOAP notes with our AI-powered tool.
How It Works
3-Step process to generate SOAP notes.
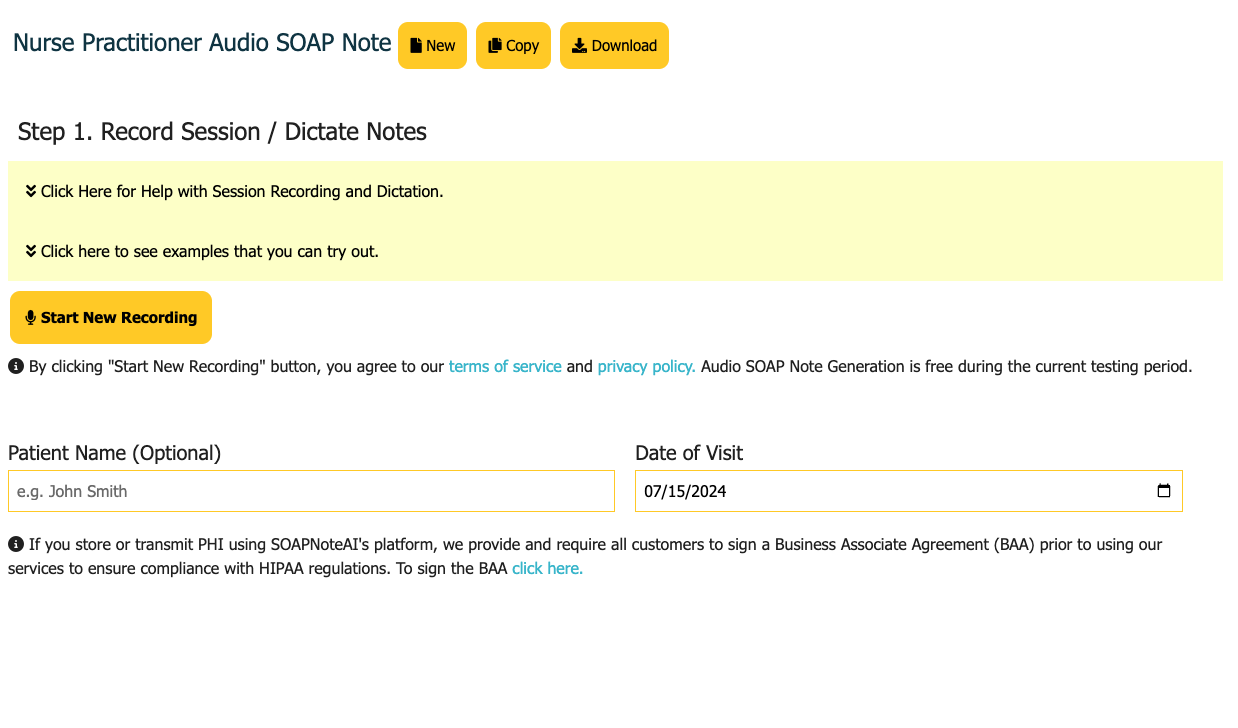
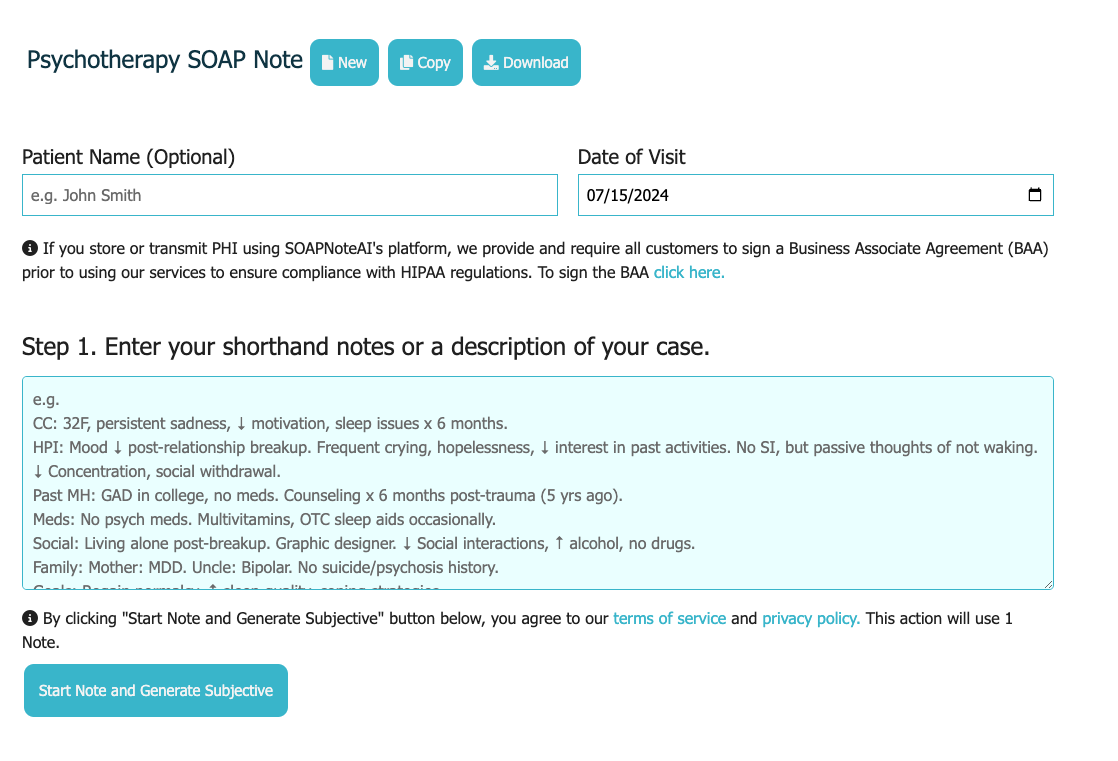
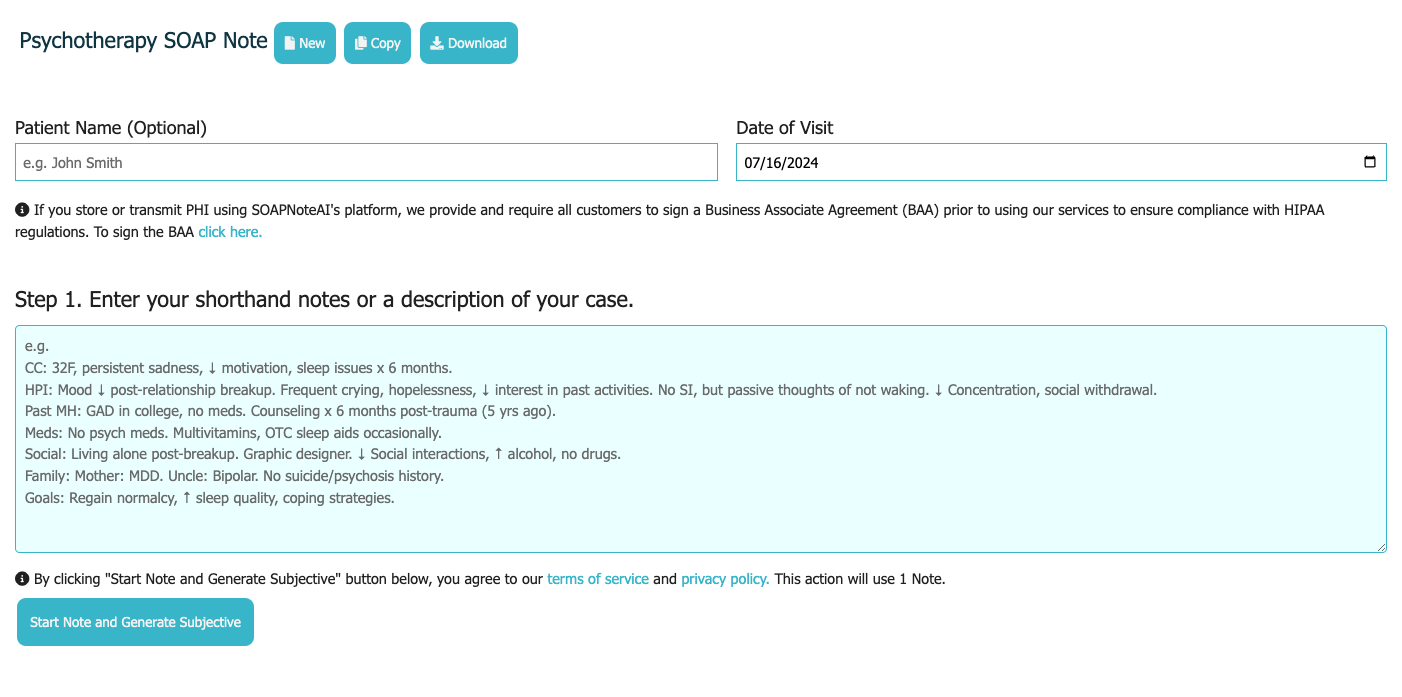
Step 1: Choose a Template
Select a template based on your profession
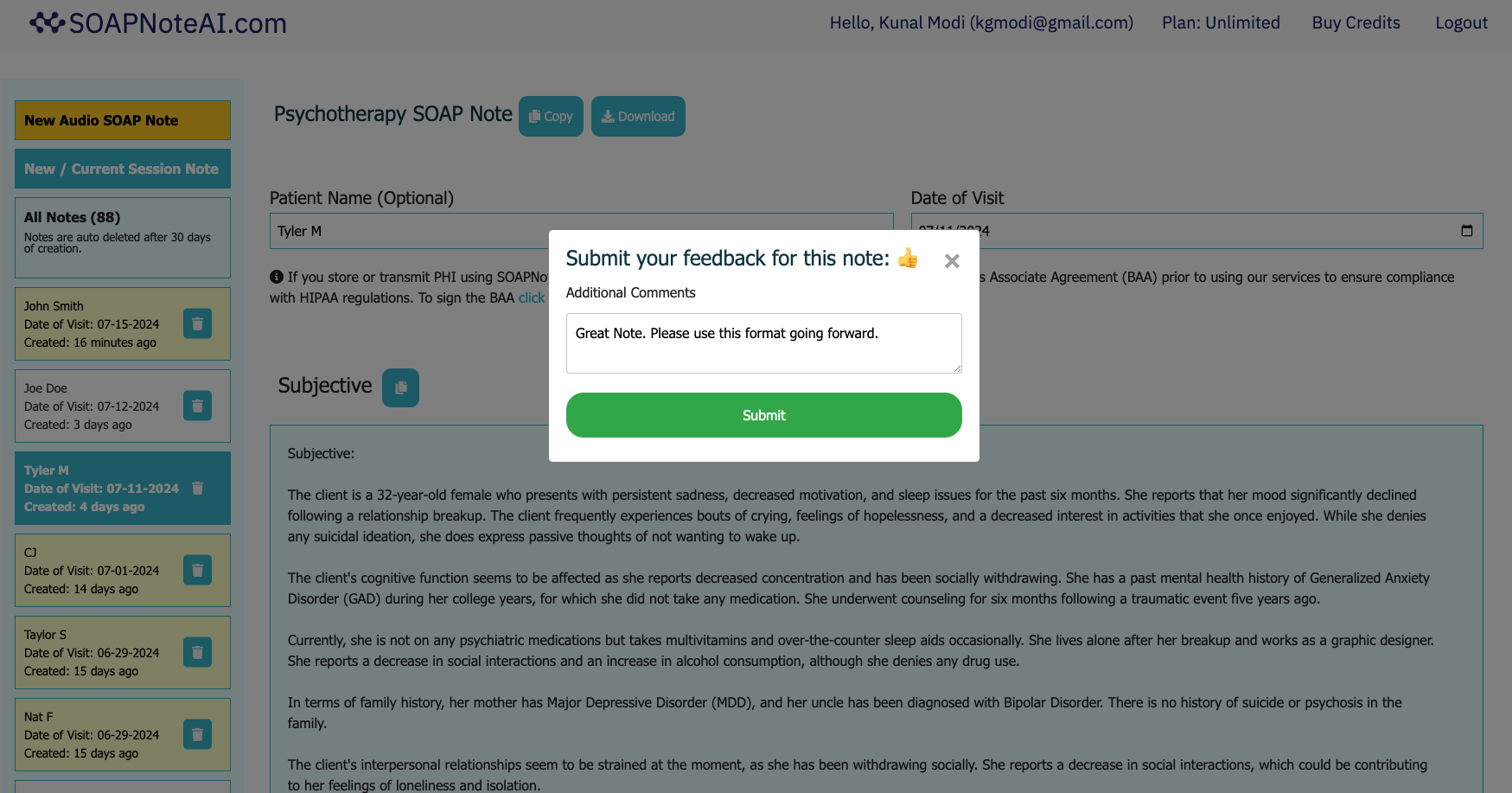
Each template is designed to capture the most relevant information for your profession. You can give feedback on the generated note. Start by selecting the SOAP note template that best fits your needs on the top of the page.
Step 2: Type / Dictate / Record
Type, dictate or record your notes
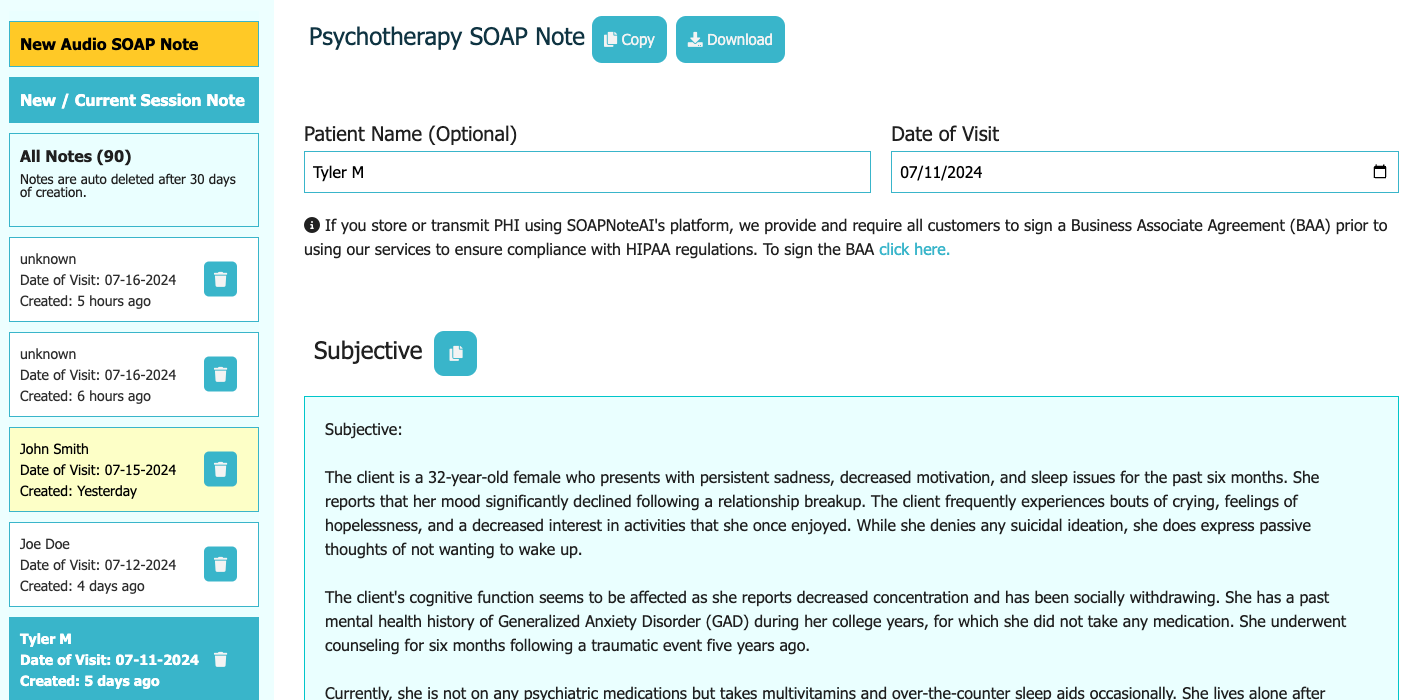
If you type, the tool will first generate the Subjective portion. Review and Edit the Subjective portion to generate the Objective portion. Repeat the process for Assessment and Plan. If you dictate or record, the tool will generate the entire note in one step.
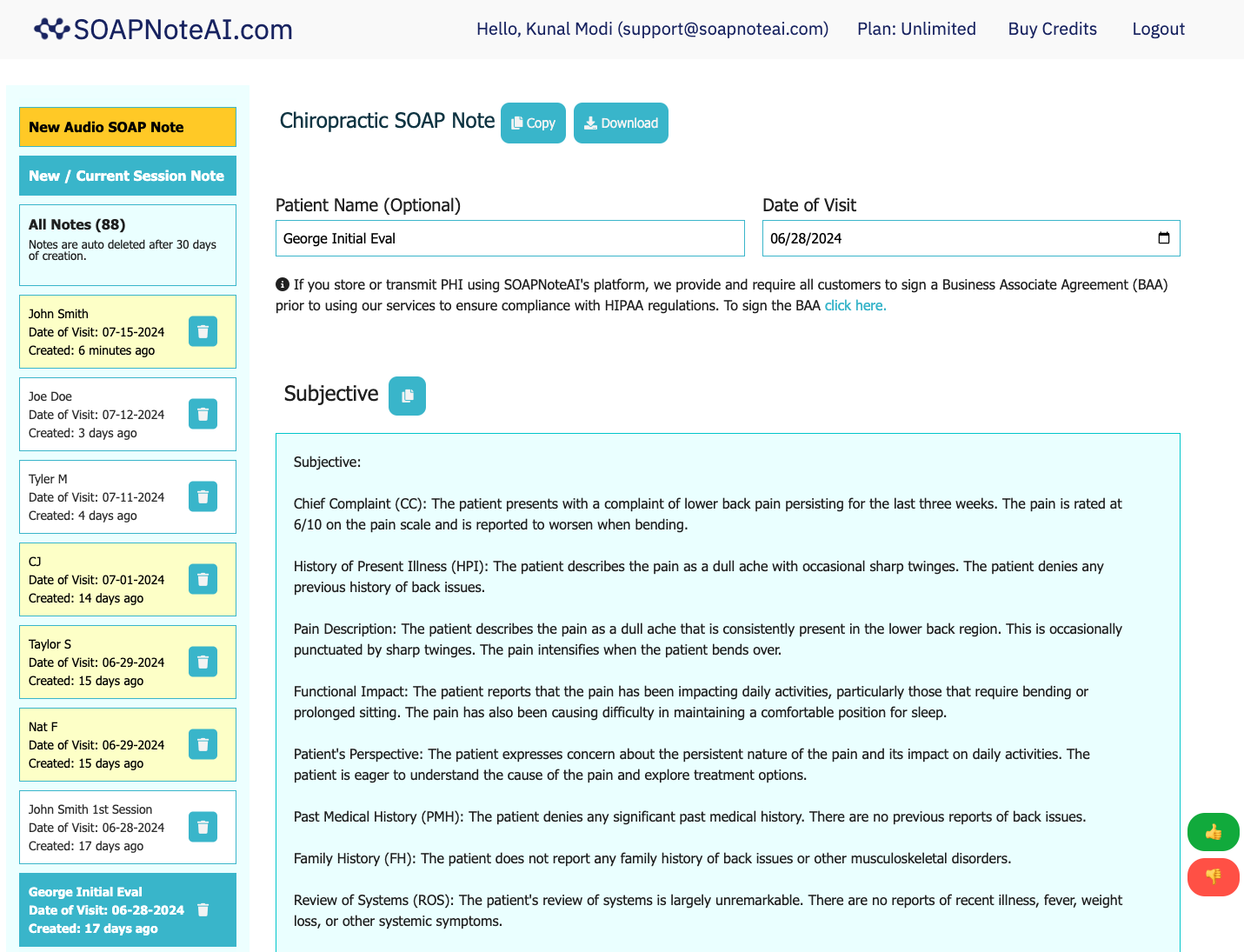
Review, Edit and Download
Review, Edit and Download your note
Review the generated note. This is an important step to ensure the note is accurate and complete. Edit the note where needed. Download the note in text format or Copy it into your EMR. All notes are available upto 30 days from the date of creation.
Select a template based on your profession
Each template is designed to capture the most relevant information for your profession. You can give feedback on the generated note. Start by selecting the SOAP note template that best fits your needs on the top of the page.
Type, dictate or record your notes
If you type, the tool will first generate the Subjective portion. Review and Edit the Subjective portion to generate the Objective portion. Repeat the process for Assessment and Plan. If you dictate or record, the tool will generate the entire note in one step.
Review, Edit and Download your note
Review the generated note. This is an important step to ensure the note is accurate and complete. Edit the note where needed. Download the note in text format or Copy it into your EMR. All notes are available upto 30 days from the date of creation.
🤖 Auto Notes That Write Themselves
Stop spending hours on documentation. Our AI automatically generates complete, compliant SOAP notes from your patient interactions in real-time.
Voice to Auto Note
Speak naturally during or after visits. AI automatically converts speech to structured SOAP format.
Text to Auto Note
Type quick shorthand notes. AI expands them into complete, professional documentation automatically.
Session to Auto Note
Record patient sessions. AI automatically transcribes and generates comprehensive SOAP notes.
2 Minutes
Average time to generate a complete auto note
vs. 30+ minutes writing manually
Specialized Solutions for Different Healthcare Professions
Learn How SOAP Note AI Can Be Useful to Your Profession
Discover how we help healthcare professionals like you save time on documentation
Therapists
AI-powered therapy notes for psychotherapists, psychiatrists, and counselors. Save hours on documentation with AI-assisted SOAP notes.
Nurse Practitioners & RNs
Specialized SOAP notes for nursing professionals. Save 1-2 hours daily on documentation.
Physical Therapists
AI-powered physical therapy notes for PTs, PTAs, and OTAs. Let notes write themselves.
Simplify Your Documentation Process
- Save Time
- Reduce your daily documentation times by up to 50%.
- Safe and Compliant
- Our technology is HIPAA-compliant and uses industry best practices.
- Generate any note
- Generate and download as many notes for your case scenarios in just a couple of minutes.
- Flexible Pricing Plans
- Subscribe Monthly or Pay-as-you-go. No hidden fees.
📋 Free SOAP Note Resources
Access professional templates and examples before you start. Copy, customize, and learn from our comprehensive documentation library.
Free SOAP Note Templates
10 professional templates ready to copy and customize. Includes Mental Health, Physical Therapy, Nursing, Primary Care, and more specialties.
- Copy & paste ready templates
- Download as PDF or text file
- 10 different healthcare specialties
- Compliance-focused formatting
Mental Health SOAP Examples
10 comprehensive mental health documentation examples including crisis intervention, therapy sessions, and medication management.
- Depression, Anxiety, PTSD examples
- Crisis intervention & suicide risk
- CBT, couples therapy sessions
- ADHD & medication management
Pricing Plans
Simple, transparent pricing
Unlimited Monthly Subscription Plans
Choose the plan that works best for you
Audio Only Plan
Generate as many audio notes - Dictation, AI Scribe and Telehealth.
$69 / month
- Generate unlimited audio notes
- Audio Dictation supported
- AI Medical Scribe / Session Recording up to 2 hours supported
- Telehealth session recording and notes supported
- Upload recordings supported
- Renews every month
- Access notes up to 30 days
- Office Hours Support
- Cancel anytime, no contract
Audio and Text Unlimited Plan
Generate as many notes - Text, Dictation, AI Scribe and Telehealth.
$79 / month
- Generate unlimited notes
- Text / Shorthand notes supported
- Audio Dictation supported
- AI Medical Scribe / Session Recording up to 2 hours supported
- Telehealth session recording and notes supported
- Upload recordings supported
- Renews every month
- Access notes up to 30 days
- Office Hours Support
- Cancel anytime, no contract
Pay As You Go Plans
Perfect for occasional use
Basic Pack
Good for providers who needs to get started with the platform.
$9
- Generate upto 10 Text SOAP notes
- $0.90 per note
- 1-year validity
- Access notes upto 30 days
- Text Shorthand SOAP Notes supported
Ultra Pack
Perfect for small businesses with unpredictable bursts of note volume.
$59
- Generate upto 100 Text SOAP notes
- Generate upto 5 Audio SOAP notes
- 1-year validity
- Access notes upto 30 days
- Text Shorthand SOAP Notes supported
- Audio SOAP Notes supported
Pro Pack
Perfect for providers with one-time need to quickly get their notes done.
$19
- Generate upto 25 Text SOAP notes
- Generate upto 3 Audio SOAP notes
- 1-year validity
- Access notes upto 30 days
- Text Shorthand SOAP Notes supported
- Audio SOAP Notes supported
If you are a student or a trainee provider, please contact us at support@soapnoteai.com for special pricing.
Frequently Asked Questions
Frequently asked questions
Below are some of the frequently asked questions about SOAPNoteAI.com. If you have any other questions, please email us at support@soapnoteai.com. We usually respond within 24 hours if not sooner.
How to generate SOAP notes using SOAPNoteAI.com?
- Step 1. Provide a high level description of your sample scenario and click 'Generate Subjective' button, or use audio dictation, AI Scribe session recording, or telehealth session recording. This will generate the Subjective Section of the SOAP note. Adjust the Subjective section by editing the generated text (add or remove text) as per your needs.
- Step 2. Once you have finalized the Subjective portion of the note, click on 'Generate Objective' button. This will generate the Objective section. Again, edit the section as per you needs. Repeat the process to generate the Assessment and the Plan sections of the note.
- Step 3. Once you have finalized the entire note, you can copy download the note as .txt file for your reference.
SOAPNoteAI.com can generate SOAP Notes for Physical Therapy, Occupational Therapy, Nursing, SLP and Mental Health. Once you select the type of SOAP Note by clicking on the button on the top, there are three simple steps to generate SOAP notes:
Can I take a look at some example SOAP Note generated by SOAPNoteAI?
Definitely. You can find already generated SOAP Note for sample case description on this page - https://www.SOAPNoteAI.com/soap-note-example.html
Is SOAPNoteAI HIPAA Compliant?
Yes. Our technology is HIPAA-compliant and uses industry best practices. We have established suitable administrative, physical, and technical safeguards to ensure the privacy and security of any personal health information (PHI) processed through our systems.
I want to sign a Business Associate Agreement (BAA) with SOAPNoteAI. Do you provide one?
Yes, we can provide a standard BAA between SOAPNoteAI (Business Associate) and You (Covered Entity). Please email us at support@soapnoteai.com to request the BAA.
Do you store my shorthand notes / description that I enter in SOAPNoteAI?
We do not store the raw information (e.g. your shorthand notes, description of the case) that you enter in the app. Generated notes are available to the users upto 30 days. They are encrypted and stored using industry-standard protocols to ensure your information is safe and confidential in our system.
What happens to my audio recordings and transcriptions?
All audio recordings and transcriptions are deleted after generating the notes within 24-48 hours.
Do you use my audio recordings / transcriptions / shorthand notes for training your AI models?
No. We do not use any user's audio recordings / transcriptions / shorthand notes for training our AI models.
I want to generate SOAP note for my medical speciality but they are not supported?
We would love to help you. Please drop us an email at support@soapnoteai.com with your use case and we will let you know when we are ready.
Do you provide an API that I can integrate in my app?
Yes. We do have an API. Please checkout https://www.soapnoteapi.com/. It supports all the major medical specialities. Email us your use case at hello@soapnoteapi.com to get access.
How can I generate effective notes?
- CC: 32F, persistent sadness, ↓ motivation, sleep issues x 6 months.
- HPI: Mood ↓ post-relationship breakup. Frequent crying, hopelessness, ↓ interest in past activities. No SI, but passive thoughts of not waking. ↓ Concentration, social withdrawal. Past MH: GAD in college, no meds. Counseling x 6 months post-trauma (5 yrs ago).
- Meds: No psych meds. Multivitamins, OTC sleep aids occasionally.
- Social: Living alone post-breakup. Graphic designer. ↓ Social interactions, ↑ alcohol, no drugs.
- Family: Mother: MDD. Uncle: Bipolar. No suicide/psychosis history.
- Goals: Regain normalcy, ↑ sleep quality, coping strategies.
To create effective notes, provide your shorthand notes and description with as much details as possible for your use-case including chief complaint, age, gender and onset of the complaint. For example,
Do you have a free trial?
Yes, you can start using SOAPNoteAI.com to generate up to 3 SOAP notes when you signup. No credit card is required to get started.
I used up a note. How did that happen?
In general, each new high-level scenario corresponds to a new note. So when you provide a high level description of your sample scenario and click 'Generate Subjective', you use up a note. Generating the subsequent sections of the same note does not use up your note credits.
I want to cancel my subscription plan. Where should I go?
SOAPNoteAI partners with Stripe.com to handle all subscription and payment processes. Please go to this link to update your subscription plan. Enter the email address you used to sign up for a subscription plan. https://billing.stripe.com/p/login/14k8zZ05M0uC2xq7ss
I have feedback / question. Where should I send my feedback / question?
Please send us an email at support@soapnoteai.com and we will get back to you.
I am looking to generate Mental Health DAP Note Templates. Can I generate one?
SOAPNoteAI supports SOAP Note structure. To generate DAP Note templates, please use DAPNotes.com to generate DAP Note templates.
Do you have an affiliate program?
Yes, we support affiliates. Please contact support@soapnoteai.com with your inquiry and we will get back to you with details about our affiliate program.
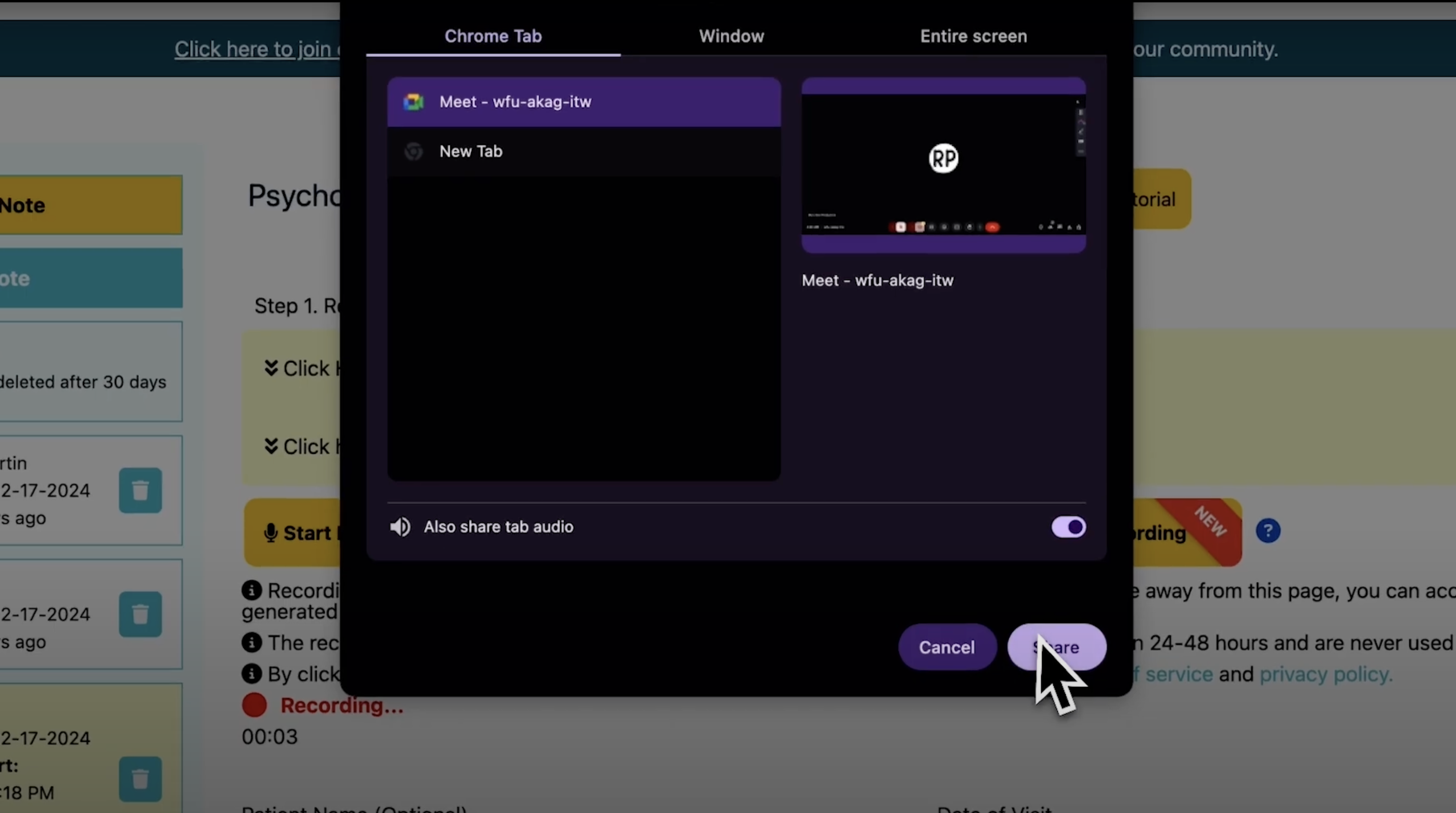
What happens to my telehealth session recordings?
Like audio recordings, all telehealth session recordings are deleted after generating the notes within 24-48 hours. We follow strict HIPAA compliance guidelines for handling all session recordings.
How do I record my telehealth sessions?
Start your telehealth session using your Chrome browser (e.g. Zoom, Google Meet, etc). Go to SOAPNoteAI.com and click 'Start New Telehealth Recording'. That's it. Please follow this video for detailed instructions - https://www.youtube.com/watch?v=5J042l14jaw
Can I generate SOAP notes from existing recordings by uploading recordings?
Yes, you can generate SOAP notes by uploading existing recordings up to 1.5 hours. Please use the Upload Existing Recording button to SOAP Note Conversion method to generate notes from your existing recordings.
Can I generate SOAP notes without recording?
Yes, you can generate SOAP notes without recording. Please use the Shorthand Text to SOAP Note Conversion method to generate notes from your existing shorthand notes.
Can I generate SOAP notes for any healthcare professions?
Yes, you can generate SOAP notes for any healthcare professions. Please go to https://www.soapnoteai.com/soap-note-generator to generate SOAP notes for any healthcare professions.
How various Healthcare Professionals use SOAP Notes
What is a SOAP Note? How do Physical Therapists use it?
- Subjective: The 'Subjective' section of the SOAP note captures information as reported by the patient. This could include the patient's reason for the visit, their perception of their health problem, the duration and intensity of their symptoms, and any relevant past medical history. In the context of physical therapy, this could be a patient describing their pain, discomfort, or difficulty in performing certain movements or tasks.
- Objective: The 'Objective' part of the note contains factual, measurable, and observable data about the patient's condition. This could include findings from the physical examination, such as heart rate, blood pressure, and other vital signs. In physical therapy, this section may also include a record of the patient's range of motion, muscle strength, posture, gait, and other functionally relevant parameters.
- Assessment: The 'Assessment' section includes the healthcare provider's professional judgment about the patient's condition, based on the information gathered in the subjective and objective sections. It may also include a diagnosis if one has been made. In physical therapy, the assessment often includes the therapist's understanding of the patient's problems and the impact of these problems on the patient's function.
- Plan: The 'Plan' is where the healthcare provider outlines the proposed course of treatment for the patient, based on their assessment. In the context of physical therapy, this may include specific exercises or interventions, the frequency and duration of therapy sessions, referrals to other healthcare providers, and goals for the patient's progress.
- Physical therapists use SOAP notes as a standardized way to document patient encounters. The structure of the SOAP note allows for clear, organized documentation of a patient's status and the care provided. It helps to ensure consistency across different providers and visits, making it easier to track a patient's progress over time. <br/> In addition, SOAP notes are often required for billing and insurance purposes. They provide proof of the care provided and justify the need for specific treatments or interventions. They also serve as a legal document, contributing to the healthcare record that can be referred to if there is ever a legal issue concerning the patient's care. <br/> In summary, a SOAP note is an essential tool for physical therapists. It facilitates effective communication among healthcare providers, supports the tracking of a patient's progress, and is critical for administrative and legal purposes.
A SOAP note is a structured form of documentation that healthcare providers, including physical therapists, use to record important details about a patient's care. The acronym `SOAP` stands for Subjective, Objective, Assessment, and Plan, which are the four sections that comprise a SOAP note. Each section serves a unique purpose in capturing comprehensive, relevant information about a patient's health status and treatment plan.
How do Occupational Therapists use SOAP Note?
- Subjective: The 'Subjective' section includes the client's feelings, perceptions, concerns, and goals related to their occupational performance. It might include quotes from the client or their family and relevant context related to the client's daily activities, work, social participation, or environment that may be impacting their function.
- Objective: This section records measurable, observable, and factual information about the client's performance and behavior during the session. Clinical findings such as range of motion, strength, coordination, and performance of specific tasks or activities are included, along with results from standardized or non-standardized assessments.
- Assessment: The OT provides an analysis of the subjective and objective information, interpreting what it means in terms of the client's occupational performance, progress, and barriers. This may include a clinical diagnosis and treatment goals, as well as updates on the client's progress toward achieving these goals.
- Plan: This section outlines the OT's plans for future treatment, including specific interventions, strategies, or modifications. It details the frequency and duration of future therapy sessions and plans for coordination with other providers if applicable.
- Additional Considerations: OTs are responsible for maintaining confidentiality and ethical standards in their documentation. SOAP notes must meet legal and insurance requirements and support interdisciplinary communication and client-centered care.
Occupational Therapists (OTs) use SOAP notes as a systematic way to document their observations, assessments, and plans for treatment. These notes are a vital part of the client's medical record and facilitate communication among various healthcare providers. Here's how OTs utilize SOAP notes:
How do Mental Health Professionals like Psychiatrists, Psychotherapists, and Clinical Social Workers use SOAP Note?
- Subjective: This is where the therapist records the patient's self-reported symptoms and feelings. It may include direct quotes from the patient, their thoughts, feelings, and perceptions. For example, a patient might express feelings of hopelessness or anxiety, and this would be noted in this section.
- Objective: This section documents measurable and observable information. In mental health settings, this could include a patient's appearance, tone of voice, or other behaviors observed during the session. If there were any assessments or tests performed, those results would also be noted here.
- Assessment: Here, the mental health professional provides a diagnosis or clinical impression based on the information gathered in the Subjective and Objective sections. It may include an analysis of the patient's progress or any challenges they are facing. This is often where the therapist will link the subjective and objective information to provide a comprehensive view of the patient's mental state.
- Plan: This section outlines the treatment plan, including any medications prescribed, therapy techniques to be used, or referrals to other specialists if needed. It provides a roadmap for how the mental health professional intends to address the issues identified in the Assessment. This may include short-term and long-term goals, frequency of therapy sessions, and any other interventions that will be used to support the patient.
- The SOAP note format offers several benefits in mental healthcare settings: consistency, communication, efficiency, legal and ethical compliance, and evaluation and adjustment.
The SOAP note (an acronym for Subjective, Objective, Assessment, and Plan) is a method used by mental health professionals, including psychiatrists, psychotherapists, and clinical social workers, to document and organize information in a patient's records. It provides a concise and standardized way to record information that is both accessible and useful in understanding a patient's status and treatment plan.
How do Nursing professionals like Registered Nurses and Nurse Practitioners use SOAP Note?
- Subjective: The nurse records information that the patient, family, or other caregivers have provided. This might include the patient's description of pain, fatigue, nausea, or other symptoms. It provides insights into how the patient is feeling and what they are experiencing from their perspective.
- Objective: In this section, the nurse includes factual, observable, and measurable data. This can encompass vital signs like blood pressure, heart rate, and temperature, as well as physical examination findings, lab results, or other diagnostic information.
- Assessment: Here, the nurse will analyze the Subjective and Objective information to form a clinical judgment. This might include identifying a specific nursing diagnosis or recognizing a change in the patient's condition that requires further intervention.
- Plan: The Plan section is used to outline the specific interventions or actions that the nurse will take to address the issues identified in the Assessment. This could include administering medications, teaching a patient about a new dietary plan, or collaborating with other healthcare professionals.
- The SOAP note format supports interprofessional communication, patient-centered care, evaluation and reassessment, legal documentation, education and training, and efficient workflow.
Nursing professionals, including Registered Nurses (RNs) and Nurse Practitioners (NPs), also utilize the SOAP note format in their practice. This approach allows for standardized documentation of patient care, aids in communication among healthcare team members, and helps in planning and evaluating patient care.
How do Speech-Language Pathologists use SOAP Note?
- Subjective: In this section, the SLP may record observations and information from the client, family, or caregivers about the individual's communication abilities, difficulties, or changes. This might include self-reported feelings about progress, frustrations with specific tasks, or anecdotal evidence of improvement or challenges outside of therapy.
- Objective: The Objective section is where the SLP records measurable and observable data collected during the session. This could include the results of specific assessments or performance on therapeutic tasks.
- Assessment: This part includes the SLP's professional judgment and analysis of the subjective and objective information. It often consists of interpretation of the data, comparison to previous sessions, or alignment with specific therapy goals.
- Plan: Finally, the Plan section outlines the future course of action for the client. This might include specific strategies to be used in the next session, adjustments to current goals, recommendations for practice at home, or referrals to other professionals if needed.
- The SOAP note format enhances client-centered care, goal tracking, interdisciplinary communication, reimbursement and legal compliance, professional reflection and growth, and family and caregiver involvement.
Speech-Language Pathologists (SLPs) also utilize SOAP notes in their practice. This standardized documentation method allows them to record, assess, and plan treatment for individuals with speech, language, voice, or fluency disorders.
How do Podiatrists use SOAP Note?
- Subjective: The podiatrist begins by gathering information from the patient about their symptoms, pain, medical history, lifestyle factors, and any other relevant details.
- Objective: Next, the podiatrist conducts a physical examination of the foot, ankle, or related areas. This may include observing the way the patient walks, checking for deformities or abnormalities, assessing range of motion, and performing specific tests. They may also review diagnostic images or lab results.
- Assessment: In this section, the podiatrist synthesizes the information gathered in the subjective and objective sections to arrive at a diagnosis or a differential diagnosis.
- Plan: The plan outlines the treatment approach and interventions that will be undertaken to address the patient's condition. This could include a combination of medications, therapies, surgical procedures, lifestyle modifications, and referrals to other specialists.
- SOAP notes provide an organized way to capture critical information about an animal's health, ensuring consistent care and effective communication among veterinary staff. They also serve as an essential record for pet owners and breeders, aiding in tracking an animal's health over its lifetime. If there's a need for legal or insurance documentation, these notes are also invaluable.
Podiatrists use SOAP (Subjective, Objective, Assessment, Plan) notes as a standardized and structured way to document patient encounters, both for initial evaluations and follow-up visits.
How do Massage Therapists use SOAP Note?
- Subjective: This is where the massage therapist records what the client reports or describes about their condition or reason for the visit. They might document any pain, discomfort, tension, or other symptoms the client is experiencing, as well as any recent injuries or significant life events.
- Objective: Here, the therapist notes their observations and findings during the session. This could include: Palpation findings, postural observations, range of motion or mobility restrictions, and any signs of swelling, discoloration, or other visible indicators.
- Assessment: The massage therapist provides their professional evaluation based on the information from the subjective and objective sections. They might note any patterns they've detected, potential causes of the client's symptoms, or how today's findings compare to previous sessions.
- Plan: This section details the therapist's plan for treatment, both for the current session and future ones. They might outline the specific techniques they intend to use, recommend the frequency of future sessions, or suggest complementary treatments or home care.
- Using SOAP notes helps massage therapists keep consistent records of their clients' conditions, their treatments, and the outcomes. This not only aids in tracking the progress of each client but also ensures a more tailored and effective treatment plan. Additionally, these notes can be crucial if a client is receiving integrated care from multiple health professionals or if there is a need to provide a history of care for insurance or other purposes.
Massage therapists use SOAP notes as a standardized method to document their treatment sessions, just as many health professionals do.
How do Veterinarians use SOAP Note?
- Subjective: In this section, veterinarians document the concerns and observations reported by the pet owner (or animal handler/keeper). Common details include the animal's behavior changes, signs of illness or distress, any noted injuries, changes in eating or drinking habits, etc.
- Objective: Here, the veterinarian records their clinical observations and findings. They document the animal's vital signs such as heart rate, respiratory rate, temperature, and weight. Physical examination findings are detailed, including the condition of the animal's coat, eyes, ears, mouth, and any noted abnormalities.
- Assessment: This section captures the veterinarian's clinical judgment or diagnosis based on the subjective history and objective findings. It's where the veterinarian might note any suspected illnesses, conditions, or injuries and how today's assessment compares with previous ones.
- Plan: Here, the veterinarian outlines their recommended course of action. They might detail specific treatments, such as medications to be administered, surgeries to be scheduled, or dietary recommendations. This section also includes recommended follow-up visits, further diagnostic tests, or referrals to specialists.
- Veterinary SOAP notes provide an organized way to capture critical information about an animal's health, ensuring consistent care and effective communication among veterinary staff. They also serve as an essential record for pet owners and breeders, aiding in tracking an animal's health over its lifetime. If there's a need for legal or insurance documentation, these notes are also invaluable.
Veterinarians, like other healthcare professionals, utilize SOAP notes as a standardized method to document and communicate about patient care.
How do Chiropractors use SOAP Note?
- Patient Care and Continuity: Tracking Progress: SOAP notes allow chiropractors to track a patient's progress over time. By documenting each visit, they can see how the patient responds to treatment and make necessary adjustments. Consistency in Care: If a patient sees multiple practitioners, SOAP notes ensure that all chiropractors are informed about the patient's condition and the treatments that have been administered.
- Clinical Decision Making: Diagnostic Tool: The Assessment section helps in forming a diagnosis based on the subjective symptoms reported by the patient and the objective findings from the examination. Treatment Planning: Based on the assessment, chiropractors develop a treatment plan, documented in the Plan section, tailored to the patient's specific needs.
- Communication with Other Healthcare Providers: SOAP notes provide a clear and concise format that can be easily shared with other healthcare providers. This is crucial for integrated care, especially if the patient is receiving treatment from multiple professionals.
- Legal and Regulatory Compliance: Record Keeping: Keeping detailed SOAP notes is a legal requirement in many regions for healthcare providers. These notes serve as a legal document that records what care was provided and why. Insurance and Billing: SOAP notes are often required for billing purposes, especially when dealing with insurance companies. They provide proof of the medical necessity of the treatment.
- Quality Assurance and Improvement: Review and Audit: Regular review of SOAP notes can help in quality assurance and in identifying areas for improvement in patient care. Educational Tool: For new practitioners or students, reviewing SOAP notes can be a valuable educational experience, aiding in understanding clinical decision-making and patient management.
Chiropractors use SOAP notes as a systematic and structured method to document patient visits and the care provided. This documentation is essential for several reasons:
How do Acupuncturists use SOAP Note?
- Subjective: Gathering information about the patient's chief complaint, symptoms, pain levels, emotional state, lifestyle factors (diet, exercise, stress), and medical history. TCM looks at the patient's overall well-being, not just isolated symptoms.
- Objective: Alongside standard physical examination findings, acupuncturists often include TCM-specific observations such as tongue diagnosis (color, shape, coating) and pulse diagnosis (quality, rhythm, strength). Palpation: Feeling the body for tender points, especially along meridian lines, and observing for any physical manifestations of Qi imbalance.
- Assessment: Integrating the subjective and objective findings to arrive at a TCM diagnosis, which typically involves identifying patterns of disharmony or imbalance (like Qi stagnation, Blood deficiency, etc.). Setting specific goals for the acupuncture treatment, such as reducing pain, improving energy levels, or balancing Yin and Yang.
- Plan: Specifying the acupuncture points to be used, the techniques (such as needling, moxibustion, cupping), and the frequency and duration of treatments. Often includes suggestions for herbal remedies, dietary changes, exercises, or lifestyle adjustments that can support the treatment.
- By using SOAP notes, acupuncturists can maintain detailed and organized records of each patient visit. This documentation is essential for tracking the patient's progress, planning and adjusting treatments, ensuring continuity of care, and communicating with other healthcare providers. SOAP notes also serve as important legal documents that record the care provided.
Acupuncturists use SOAP notes as a structured method to document patient visits and treatments, similar to other healthcare professionals, but with a focus on principles specific to Traditional Chinese Medicine (TCM) and acupuncture.
How do Pharmacists use SOAP Note?
- Subjective: Information from the patient or their medical records about the chief complaint, symptoms, medication history, adherence to therapy, any side effects experienced, and lifestyle factors that might impact medication use. Understanding the patient's perceptions and expectations regarding their medication therapy, as well as any barriers to adherence.
- Objective: Verification of the patient's current medication list, including prescription drugs, over-the-counter medications, and supplements. Relevant laboratory values, vital signs, and diagnostic test results that can influence medication therapy.
- Assessment: Evaluating the appropriateness, effectiveness, and safety of the patient's current medication regimen, and identifying any medication-related problems. Weighing the risks and benefits of the current medication therapy and considering any necessary changes. Determining if the patient's therapeutic goals are being met and setting new goals as needed.
- Plan: Adjustments to the medication regimen, such as changes in dosages, adding or discontinuing medications, and managing drug interactions or side effects. Outlining how the patient's response to medication will be monitored, including follow-up appointments and necessary laboratory tests. Providing education about proper medication use, potential side effects, lifestyle modifications, and adherence strategies.
- Pharmacists use SOAP notes as a critical tool for documenting the rationale behind medication recommendations and interventions, ensuring effective communication with other healthcare providers, and providing a structured approach to patient-centered care. This documentation is essential in both community and clinical pharmacy settings.
Pharmacists use SOAP notes to document clinical interventions, medication therapy management, and patient consultations. While the structure of SOAP notes for pharmacists is similar to that used by other healthcare professionals, the focus is tailored to medication-related aspects.
How do Dentists use SOAP Note?
- Subjective: In this section, dentists document information reported by the patient. This includes the patient's chief complaint, history of present illness, and any relevant medical or dental history. For example, a patient might report a toothache, sensitivity to hot or cold, or discomfort while chewing.
- Objective: The objective section contains the dentist's observations and findings from the clinical examination and diagnostic tests. This includes visual inspection of the teeth and gums, palpation, percussion, and results from diagnostic tools such as X-rays or other imaging studies.
- Assessment: In the assessment section, the dentist provides a diagnosis based on the subjective and objective information. This might include identifying specific dental issues such as cavities, gingivitis, periodontitis, or occlusal problems.
- Plan: The plan section outlines the proposed treatment plan to address the patient's dental issues. This includes recommended procedures such as fillings, root canals, extractions, scaling and root planing, or restorative work like crowns or bridges. The plan also details the frequency and sequence of treatments, follow-up visits, patient education on oral hygiene practices, and any referrals to specialists if necessary.
- SOAP notes are vital for tracking patient progress, ensuring continuity of care, fulfilling legal and regulatory requirements, and facilitating communication among dental and other healthcare professionals. They also support billing and insurance claims by providing detailed documentation of the care provided.
Dentists use SOAP notes as a standardized and structured method to document patient encounters, ensuring comprehensive and consistent records. This approach aids in patient care, legal documentation, and communication among healthcare providers.